Return to Normal After COVID
It’s been a little over a month since my onset of COVID and I feel that an update is needed. During this time, I’ve had many patients approach me about their experience. I’ve listened to how the it affected their health from fevers to shortness of breath. Fortunately our innate healing ability limits most of the response to short-term effects, but the life altering effects of long-haul COVID symptoms are especially touching. Dealing with continuous brain fog and chronic fatigue leads to days if not weeks of missed work, altered relationships, and loss of joy. For those dealing with these issues, my hope is that this will help you seek wellness methods to strengthening and improving your system.
My last article was written just shy of three weeks post infection. My system was depleted, but recovering at a healthy pace. I shared data that showed how my stress and body battery were altered and how my system remained weaker than before the infection. Over this three weeks time, I knew to rest and carry on with the therapies of red light, microcurrent, oxygen therapy, gentle stretching, and mental stress management. I have not deviated from the holistic nutrition plan I laid out in the last article. In fact, I’ve had a number of patients start up similar plans to help improve their recovery.
As I sit here sipping on Pine Needle tea, I am happy to report just a few days after I released the last article I began to feel like myself again. Energy levels came up, sleep improved, stress stayed low, and brain fog evaporated. At the time of writing, it has been a little over four weeks. I’ve managed to make two ten-hour driving hour trips, spend all day at a football game, attend a continuing education conference, and resume regular moderate intensity exercise.
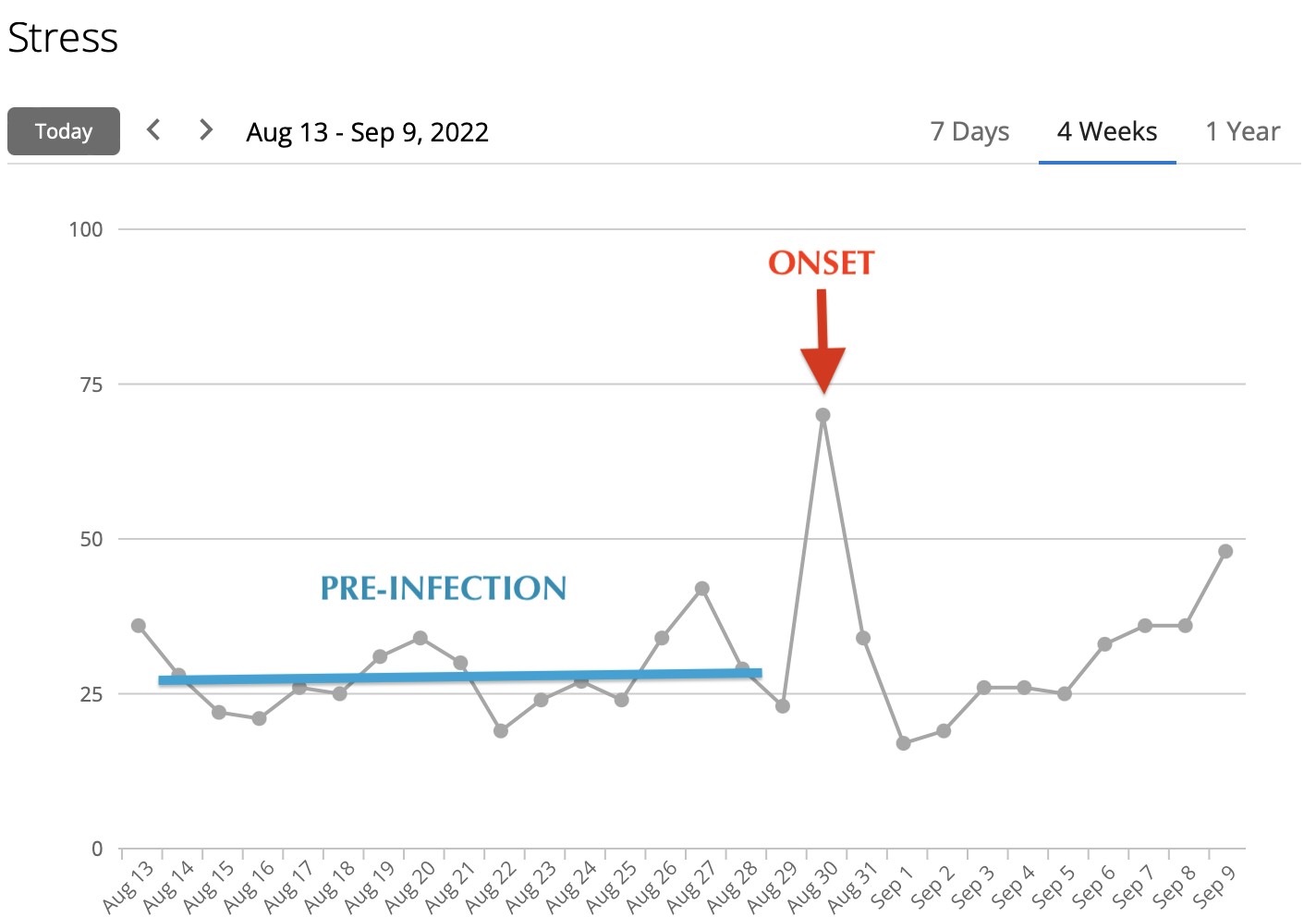
With this increased activity and a more intense work schedule, it is interesting to see that the overall trend of stress has significantly dropped. Prior to infection, my stress level averaged 26. Immediately after onset there was a spike then a drop due to medications and artifacts (I removed my watch for several hours) followed by an elevated stress response. From early September on you can see a slow drop in the daily stress level from mid 40s to 26, my typical baseline.
Like many of you, there are still limitations that I am experiencing since the onset. I fatigue more easily at work. My running capacity is reduced; running three miles is more of a challenge than it used to be and I’ve not been motivated to push into a long run. My active heart rate is higher and I’ve lost a point on my VO2max (how well the body utilizes oxygen). I’m confident these will return back to normal with proper training and time.
Hopefully, what I see in my data can help you better understand some of the body’s responses to a COVID infection. I empathize with anyone going through the residuals of COVID. My advice to you is:
Your health should be able to return to a healthy state within a reasonable period of time. If not, the limiting factor needs to be investigated and an individualized treatment plan needs to be developed.
Expect to have residuals for a while. Your body needs time to heal. Give your innate healing the time and resources it needs during this period.
Your work, activities of daily living, and exercise performance including walking, may be reduced for a while until you regrow the capacity.
If you need help setting up a plan to reinvigorate your health, please reach out to your provider or schedule a consultation with me at (304) 933-9355.
James Leonette, DC MS